Living with terminal illness in Peterborough exposes the real cost of rural healthcare access in regional South Australia
Living in the country shouldn’t mean dying without choice, dignity, or medical care. Yet for people facing serious illness, rural healthcare access in regional South Australia often falls short when it matters most. For Lou Papps, that’s a reality she lives with every day.
“I’ve nursed far too many dying people. Nobody wants to see people suffer.”
Lou is 64. She lives with emphysema and myeloma, an incurable blood cancer. She knows her time is limited. What frightens her most isn’t death. It’s what happens when you’re seriously ill in a town without doctors.
“We’ve got no medical centre. That’s just made it ten times worse,” she says. “It’s a knock-on effect that affects everybody.”
Lou has watched people in rural towns die alone. Undiscovered for days. Not because family didn’t care, but because healthcare access failed them.
“That’s what happens when seriously ill people live alone and can’t see doctors,” she says.
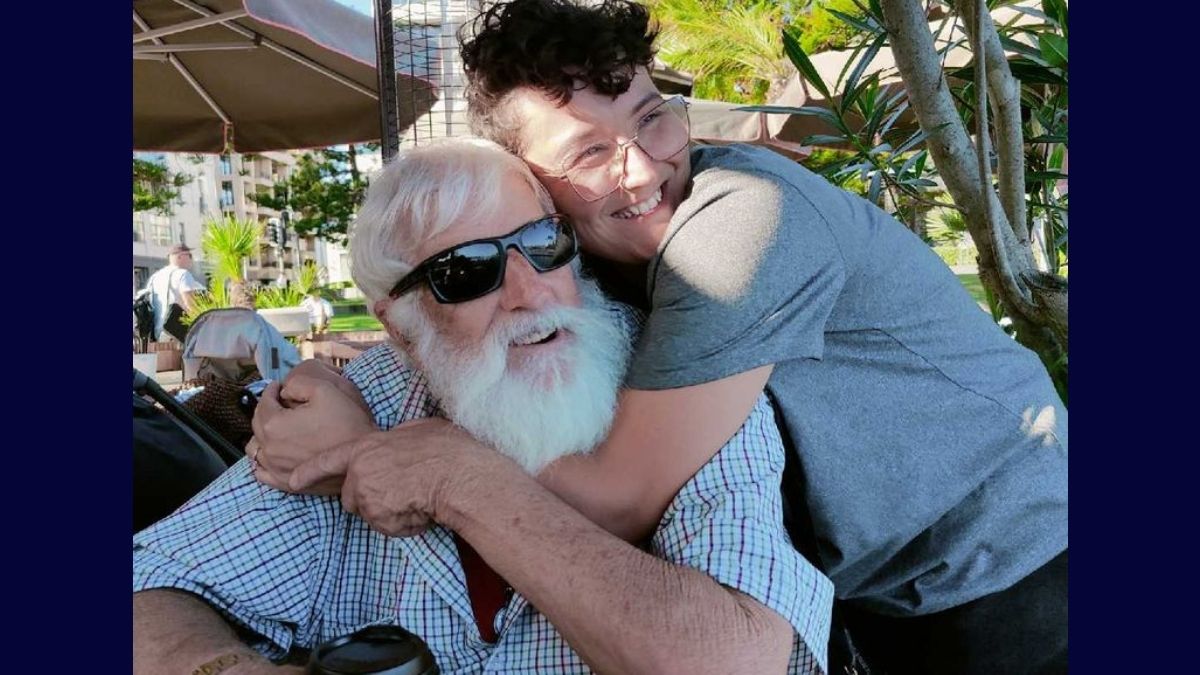
Independence matters to Lou. She refused her son’s offer to move to Adelaide full-time, joking she would “cramp his dating style.” But during her stem cell transplant recovery in early 2024, she stayed with him out of necessity. With no permanent doctors at the Peterborough Hospital, any post-transplant complication would have required urgent access to specialist care well beyond what was available locally.
Now, managing illness means managing distance.
Every Monday, Lou drives herself to Jamestown for routine blood tests. One hour round trip. The alternative is waiting for hours in Peterborough Hospital’s emergency department.
“I could be there four or five hours just to get my bloods done,” she says. “And it’s not their fault. The permanent staff are under so much pressure.”
Fridays bring chemotherapy in Port Pirie. Three hours on the road, every week.
“Some days I’m on autopilot behind the wheel,” she says. “Which is probably dangerous.”
Lou moved to Peterborough in 2021 after living on Lamb Island in Queensland and in Tasmania. A budget-friendly property search brought the former aged care and disability worker to the Mid North.
“It’s a lovely community. Everyone keeps an eye on everybody,” she says. “It’s home.”
She’s seen the town rally around its own, including supporting a close friend who chose voluntary assisted dying at Peterborough Hospital.
“We had the best day with her family,” Lou says. “And I’ve never laughed so much in all my life because she was a character. It was a lovely memory.”
But her nursing background makes the system failures impossible to ignore.
“Our health system can’t keep up with these chronically unwell people,” she says. “If there were real incentives for doctors to work in regional towns, it would help everyone, including the city system.”
Lou worries about what comes next for towns like hers.
“We’re an older population and this is only going to get worse,” she says. “Just because we’re little, it doesn’t mean we don’t exist. We all exist. And it’s a beautiful town.”
This is the third story in the From Here to Healthcare series, a grassroots storytelling initiative led by Alex Thomas and supported by Greater SA. The series shares real experiences from country South Australians to show how access to healthcare changes lives, and outcomes, based on postcode alone.
Want more South Aussie stories like this? Subscribe here for free